January exam
QUESTION NO1)
1) ? SLE INDUCED ENCEPALITIS
2) ? ACUTE MENINGITIS
3) ? SIADH
4) ? ACUTE CVA
B) Neuropsychiatric syndromes vth sle
· Aseptic Meningitis
o Stroke o Transient Ischemic Attack o Cerebral Venous Sinus Thrombosis · Cognitive Disorders o Delirium (Acute confusional state) o Dementia o Mild Cognitive Imapirment · Demyelinating syndromes · Headaches o Tension Headaches o Migraine Headaches
|
The pathogenic etiologies of NPSLE manifestations are likely to be multifactorial and may involve autoantibody production, microangiopathy, intrathecal production of proinflammatory cytokines and premature atherosclerosis .
Cellular and parenchymal changes in lupus murine models include neuronal cytotoxicity and atrophy of dendritic spines . Cerebral spinal fluid from lupus-prone mice and adult patients with NPSLE reduce the viability of proliferating neural cells lines .
Postmortem histopathologic studies reveal a wide range of brain abnormalities caused by multifocal microinfarcts, cortical atrophy, gross infarcts, hemorrhage, ischemic demyelination and patchy multiple-sclerosis-like demyelination in people with SLE .
A microvasculopathy which was formerly attributed to deposition of immune complexes but now is suspected to arise from activation of complement, appears to be the most common microscopic brain findings in SLE . Consistent with these small vessel changes, SPECT and MR spectroscopy studies suggest that both cerebral atrophy and cognitive dysfunction in SLE patients may be related to chronic diffuse cerebral ischemia.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2981505/
As pt is having euvolemic hyponatremia could be due to siadh which is due to infection(? meningitis)
pt having neck rigidity,fever,headche,vomitings MRI brain and LUMBAR PUNCTURE SHOULD BE PLANNED TO RULE OUT MENINGITIS.
O/e pt is having dec power of upperlimbs vth exggerated reflexes CVA should be ruled out.
sle and hyponatremia:
We found that hyponatremia was associated with increased ESR, CRP, and SLEDAI and decreased serum albumin and C3 levels by various statistical methods (univariate, multivariate and correlation analyses) in our cohorts of SLE, suggesting that hyponatremia in SLE is closely related to more severe inflammation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4872139/
Patients and Methods: A total of 101 patients with SLE were enrolled in this study and divided into two groups according to Na level; a normo-natremic group and a hyponatremic group. Demographic and clinical data were collected. SLE activity was assessed by the systemic lupus erythematosus disease activity index (SLEDAI). The estimated sedimentation rate (ESR) as well as levels of C-reactive protein (CRP) and complements (C3 and C4) were measured.
Results: The majority of patients were females (98 subjects) (97%) with a mean age of 33± 8 years. Out of 101 participants, 40 patients (39.6%) were hyponatremic with a mean Na level of 131.58± 3.11 mmol/L. There was a statistically negative correlation between both ESR and SLEADI score and Na level (r=− 0.436 and − 0.436, respectively) with p=0.002, whereas Na level was positively correlated with complements, Cl, and albumin levels (r=0.653, 0.314, and 0.460, respectively) (p=0.000, 0.027, and > 0.001, respectively). CRP was not correlated with Na level. ESR was independently correlated with hyponatremia at the 95% CI for Exp B (0.997– 0.058) with a p-value of 0.048.
Steroid medications work quickly to decrease the swelling, warmth, tenderness and pain that are related to inflammation. They do this by lessening the immune system's response. Prednisone is the most commonly prescribed steroid for lupus.
hcq in sle:-https://pubmed.ncbi.nlm.nih.gov/29987550/#:~:text=Conclusio
Background: Hydroxychloroquine (HCQ) is a widely prescribed medication to patients with systemic lupus erythematosus (SLE), with potential anti-inflammatory effects. This study was performed to investigate the efficacy of HCQ therapy by serial assessment of disease activity and serum levels of proinflammatory cytokines in SLE patients.
Methods: In this prospective cohort study, 41 newly diagnosed SLE patients receiving 400 mg HCQ per day were included. Patients requiring statins and immunosuppressive drugs except prednisolone at doses lower than 10 mg/day were excluded. Outcome measures were assessed before commencement of HCQ therapy (baseline visit) as well as in two follow-up visits (1 and 2 months after beginning the HCQ therapy). Serum samples of 41 age-matched healthy donors were used as controls.
Results: Median levels of IL-1β (p < 0.001), IL-6 (p = 0.001), and TNF-α (p < 0.001) were significantly higher, whereas, median CH50 level was significantly lower (p < 0.001) in SLE patients compared with controls. Two-month treatment with HCQ resulted in significant decrease in SLEDAI-2K (p < 0.001), anti-dsDNA (p < 0.001), IL-1β (p = 0.003), IL-6 (p < 0.001) and TNF-α (p < 0.001) and a significant increase in CH50 levels (p = 0.012). The reductions in SLEDAI-2K and serum levels of IL-1β and TNF-α were significantly greater in the first month compared with the reductions in the second month.
Conclusion: HCQ therapy is effective on clinical improvement of SLE patients through interfering with inflammatory signaling pathways, reducing anti-DNA autoantibodies and normalizing the complement activity.
sulfasalazine is usually not prescribed in sle as it cause drug induced sle.
E) ANA sensitivity time diagnose sle :- ANA titer of 1:40 or higher is considered positive. An ANA titer of less than 1:40 is useful for ruling out SLE in children (sensitivity of 98%). A repeated negative result makes a diagnosis of SLE unlikely but not impossible. The ANA titer does not correlate with the severity of the disease.
Objective: To determine the sensitivity and specificity of ANA and anti-dsDNA in SLE patients, using sera from HC and MMP patients.
Methods: Serum samples from HC, MMP and SLE patients, 100 in each group, were analyzed for the presence of ANA and anti-dsDNA, by indirect immunofluorescent assay, using a HEp-2 cell and Crithidia luciliae as substrates, respectively.
Cardiovascular.
In a study that involved 19 normotensive individuals without diabetes, 17 hypertensive individuals without diabetes, and 6 hypertensive individuals with diabetes, Resnick et al. documented the lowest mean intracellular Mg concentration among the last group. Similarly, based on data from the Atherosclerosis Risk in Communities (ARIC) Study, a multicenter, prospective cohort study that lasted 4 to 7 yr and involved 13,922 middle-aged adults who were free of coronary heart disease at baseline, an inverse association between serum Mg and the risk for coronary heart disease was observed among men with diabetes
Diabetic Retinopathy.
The link between hypomagnesemia and diabetic retinopathy was reported in two cross-sectional studies that involved both “insulin-dependent” patients and patients with type 2 diabetes. Not only did patients with diabetes have lower serum Mg levels compared with their counterparts without diabetes, but also the serum Mg levels among the cohort with diabetes had an inverse correlation with the degree of retinopathy A similar link, however, was not observed when Mg was measured within mononuclear cells. In a study that involved 128 patients with type 2 diabetes and poor glycemic control (glycosylated hemoglobin >8.0%), intramononuclear Mg concentrations were not observed to be lower among those with diabetic retinopathy but rather among those with neuropathy and coronary disease .
Foot Ulcerations.
Given the link between hypomagnesemia and risk factors for the development of diabetic foot ulcers(e.g., polyneuropathy, platelet dysfunction), Rodriguez-Moran and Guerrero-Romero ( suggested that hypomagnesemia may be associated with an increased risk of diabetic foot ulcers. Indeed, they observed a higher incidence of hypomagnesemia among their patients with diabetic foot ulcers compared with those without the condition (93.9% of the 33 patients with diabetic foot ulcers compared with 73.1% of the 66 patients without diabetic foot ulcers; P = 0.02).
Nephropathy.
In a comparative study that involved 30 patients who had type 2 diabetes without microalbuminuria, 30 with microalbuminuria, and 30 with overt proteinuria, Corsonello et al. observed a significant decrease in serum ionized Mg in both the microalbuminuria and overt proteinuria groups compared with the nonmicroalbuminuric group. Accordingly, in a recent retrospective study, an association between low serum Mg levels and a significantly faster rate of renal function deterioration in patients with type 2 diabetes was reported
In a large prospective cohort study, we demonstrate a consistent relationship between estimated urinary sodium excretion as a marker of sodium intake and elevation in blood pressure. These relationships were present both in the whole cohort and when restricted to subjects free of baseline comorbidity, specified by restricting analysis to those without baseline CVD, DM, or treated hypertension and with Charlson comorbidity score of zero. These findings are consistent with other cohort studies, interventional clinical trials, and meta-analyses.
The mechanisms by which dietary sodium contributes to raised blood pressure have been reviewed extensively elsewhere. Sodium excess has been associated with excess activation of the sympathetic nervous system, increased vascular tone, and endothelial dysfunction, as well as end organ damage with left ventricular hypertrophy, glomerulosclerosis, and arteriolosclerosis. In industrialized countries, diets rich in sodium and low in potassium are the norm. Processed meals are rich in sodium. Societies following a nonindustrialized diet low in sodium have low prevalence (<1%) of hypertension. Meta-analyses demonstrate that reduction in dietary sodium intake is associated with average reduction in systolic blood pressure of 3 to 5.4 mm Hg in hypertensive subjects. Our data add weight to the hypothesis that reduction of dietary sodium intake may lead to lower blood pressure. Unfortunately, we do not have long-term blood pressure changes to assess the influence of sodium intake on development of hypertension
https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.119.12726
QUESTION NO3)
P-Patients with ischaemic stroke but not complete paresis were included. No antiplatelet drugs were allowed within the last 72 h before onset. Delay until first trial dosage was maximized to 48HR.
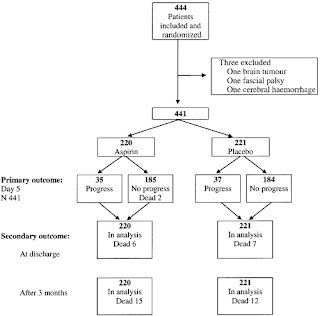
Totally, 441 patients (220 aspirin, 221 placebo) completed the trial.
I- Aspirin (325 mg) or placebo was given once daily for five consecutive days.
C-Neurological assessments were carried out three times daily during the treatment period to detect progression of at least two points in the Scandinavian Stroke Supervision Scale. Patient outcome was followed up at discharge and at 3months.
Tablets of 325 mg aspirin or placebo, water solvable, were administered orally once a day for five consecutive days. The first dosage was given as soon as possible after inclusion. The trial treatment was discontinued if the main outcome event occurred, i.e. progression of stroke symptoms.
O- The main results of the trial showed that aspirin treatment did not significantly reduce the rate of stroke progression. the progression rate was 15.9% amongst patients treated with aspirin and 16.7% for those on placebo





Comments
Post a Comment